1 in 10 women in the U.S. has polycystic ovary syndrome (PCOS), making it one of the most common hormonal conditions affecting women today. That said, PCOS could be even more prevalent than we think. Experts estimate up to 70% of Cysters go undiagnosed. It’s a pretty shocking statistic! And it’s heartbreaking to think how many women are struggling with symptoms that could be reversed if they only knew what was going on.
PCOS often goes undiagnosed simply because of a lack of knowledge. Most doctors aren’t super well-educated on the condition and, even if they were, no single test can definitively diagnose you. On top of that, women are often told their symptoms are normal, in their head, or simply due to stress, weight, or crappy sleep.
As a Cyster myself and a PCOS dietitian, I want to help other women get diagnosed, understand their condition, and find natural healing. So, in this post, I’m going to get into it all! I’ll explain what PCOS is, where it comes from, and how you can reverse your symptoms.
Here’s what you need to know:
What is PCOS or Polycystic Ovarian Syndrome?
Polycystic ovarian syndrome (PCOS) is a chronic hormonal and metabolic condition. It affects women of reproductive age and usually involves three main root issues: insulin resistance, inflammation, and hormonal imbalance. Because these problems can impact the body in so many ways, PCOS looks a little different for every Cyster.
Note: Polycystic ovary syndrome is actually a terrible name for this condition. Initially, doctors thought the trademark symptom of PCOS was cysts on the ovaries. However, many women with PCOS don’t ever have cysts! So, don’t let the name fool you. Even without cystic ovaries, you could still have PCOS.
When Does PCOS Develop?
PCOS usually pops up around puberty. That said, this isn’t true for everyone—sometimes symptoms don’t become obvious until later in life. A few early signs of PCOS during puberty include:
- Irregular or very painful periods
- Persistent acne
- Rapid weight gain (and can’t lose weight)
- Excess hair growth on the face and body
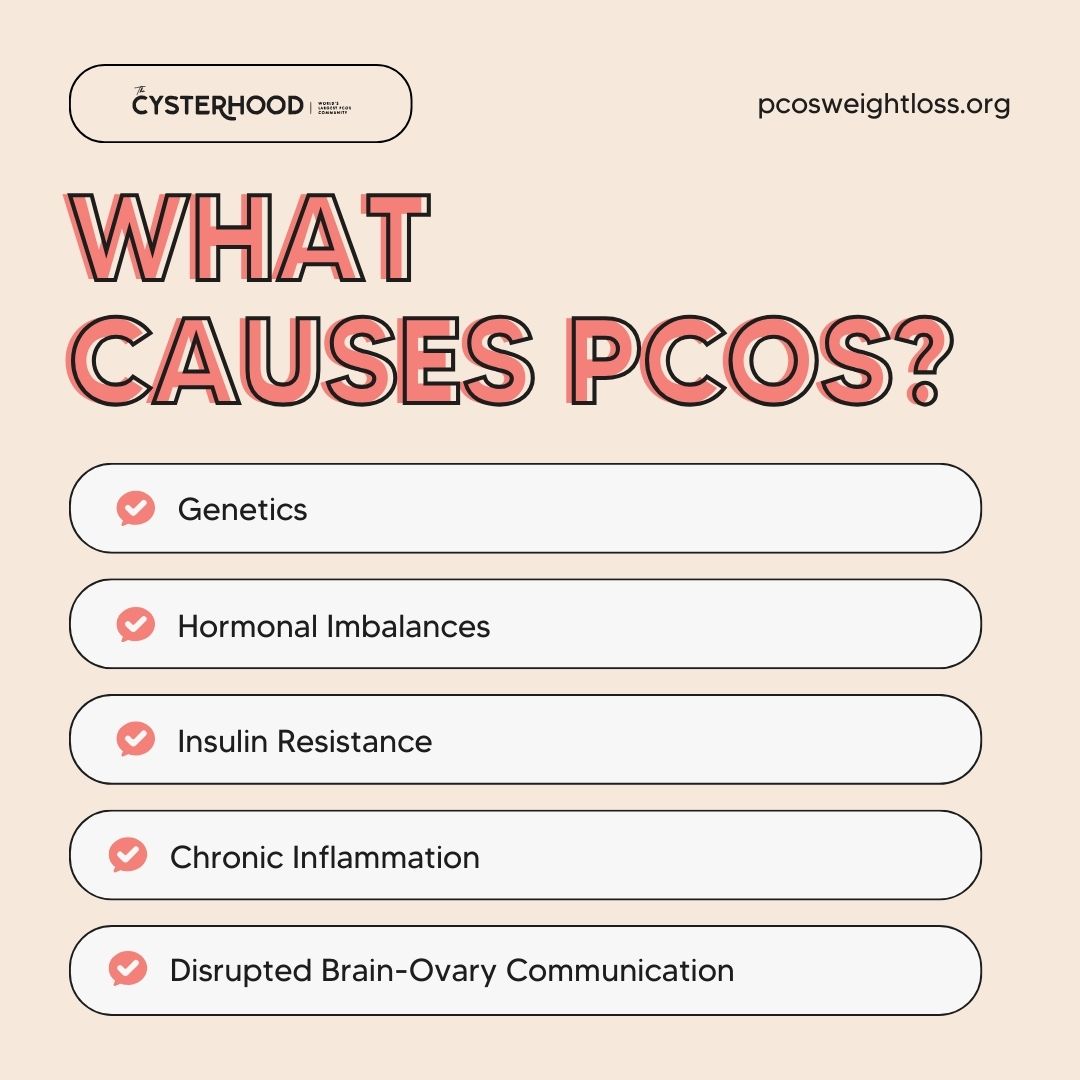
What Causes PCOS?
Genetics
Genetics definitely play a role in PCOS—a pretty big one, actually! Between 20-40% of Cysters have a close female relative with PCOS or related health problems. A family history of Type 2 diabetes, metabolic syndrome, obesity, and autoimmune disease can all increase your chances of having PCOS as well.
Hormonal Imbalances
At its core, PCOS is a hormonal condition, and imbalanced hormone levels are one of the main triggers for symptoms. Think of hormones like messengers that tell our whole body what to do. When there’s dysregulation, the side effects can quickly become overwhelming—and pop up throughout your entire body. Here are some common hormonal imbalances you’ll find with PCOS:
Insulin Resistance
Up to 80% of women with PCOS have insulin resistance. This is when your body doesn’t respond to glucose properly. Instead of converting sugar to energy, it’s stored as fat and absorbed into the bloodstream. This causes a lot of metabolic and hormonal problems and a long list of symptoms.
To learn more, listen to this episode of A Cyster & Her Mister, “Reversing Insulin Resistance with PCOS!”
Chronic Inflammation
Some doctors theorize that PCOS may be an autoimmune disease. They’re very common in women and seem to be linked to problems in the reproductive system. More specifically, many Cysters have chronic, low-grade inflammation, like those with an autoimmune disease.
It means their immune system is constantly activated, which, over time, can cause disruption all throughout the body. It can even worsen insulin resistance and hormonal balance. Inflammation, insulin resistance, and hormonal imbalance all feed into each other in a vicious, exhausting cycle.
Disrupted Brain-Ovary Communication
PCOS can also involve disrupted communication between the brain and the ovaries. Normally, the brain sends balanced hormonal signals to the ovaries, telling them when to ovulate and how much estrogen and progesterone to produce. With PCOS, these signals can become out of rhythm.
When this happens, the ovaries may produce high levels of androgens while ovulation becomes irregular or stops altogether. This leads to low progesterone and contributes to common PCOS symptoms like irregular periods, acne, hair changes, and fertility challenges. Insulin resistance and chronic inflammation can worsen this signaling issue, reinforcing the hormone imbalances seen in PCOS.
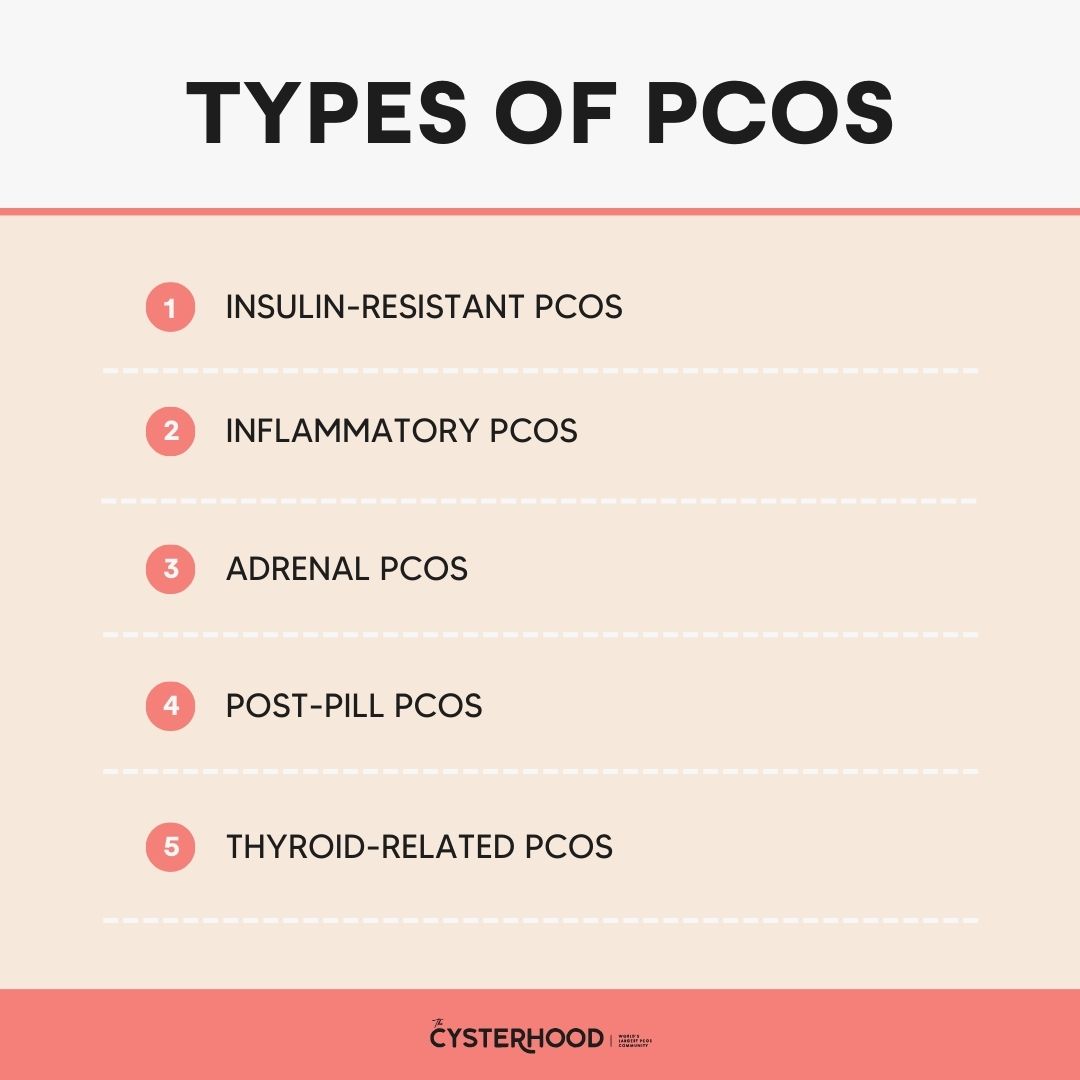
Types of PCOS
As you research your condition, you’ll find a few main “types of PCOS.” These aren’t hard and fast categories, and most women won’t perfectly fit in any one box. However, knowing your PCOS type helps you understand the core issue driving most of your symptoms. That way, you can target that primary problem first!
Below, I’ll explain each category in more depth. However, make sure you take this PCOS type quiz, too.
Insulin-Resistant PCOS
This is the most common PCOS type, and it’s driven by blood sugar dysregulation. You may have insulin-resistant PCOS if you deal with stubborn weight gain (especially belly weight), intense sugar/carb cravings, feeling hungry soon after eating, fatigue after meals, skin darkening (acanthosis nigricans), or skin tags. A doctor can help confirm it with labs like fasting insulin, glucose/A1C, or an oral glucose tolerance test.
Learn more about stubborn weight gain in my post, “What Is PCOS Belly?”
Inflammatory PCOS
Inflammatory PCOS occurs when chronic, low-grade inflammation is a major driver of your symptoms. You may have this type if you experience bloating, puffiness, cystic acne, rashes, joint aches, brain fog, fatigue, or a weight loss plateau. This is especially true if symptoms flare after certain foods (common culprits are gluten/dairy for many Cysters). Lab clues can include markers like C-reactive protein (CRP), along with your symptom patterns and food sensitivities.
Adrenal PCOS
Adrenal PCOS is tied to stress hormones and an overworked nervous system. You may have this type if your symptoms worsen during stressful seasons of life. Other common symptoms include chronic fatigue, anxiety, trouble sleeping, feeling “wired but tired,” and irregular cycles. And, similar to insulin-resistant PCOS, you may also deal with weight retention that gets worse with intense workouts or restrictive dieting.
It’s often identified by your symptom pattern and cortisol/stress markers (with your doctor), and by noticing how your body responds to rest, sleep, and low-impact movement.
Post-Pill PCOS
Post-pill PCOS refers to PCOS-like symptoms that appear after stopping hormonal birth control. Birth control suppresses ovulation and alters natural hormone signaling. When you discontinue it, the body has to relearn how to regulate hormones and cycles on its own. For some women, this transition is smooth. But for others, underlying issues like insulin resistance or inflammation surface once the pill is no longer masking symptoms.
You may have post-pill PCOS if your periods don’t return within a few months, or you notice new or worsening acne, hair shedding, mood swings, weight gain, or cycle irregularity after stopping birth control. This type is often identified by timing—symptoms that began after discontinuing the pill rather than earlier in life. Additionally, it typically improves as hormone signaling stabilizes with the right support.
Note: People also often wonder if you can get PCOS after having kids. The short answer is no, but read my post: “Can You Develop PCOS After Pregnancy?” for more details.
Thyroid-Related PCOS
Thyroid-related PCOS occurs when thyroid dysfunction contributes to or worsens PCOS symptoms. The thyroid plays a major role in metabolism, ovulation, and hormone regulation. As a result, even subtle thyroid imbalances can disrupt menstrual cycles and amplify androgen-related symptoms.
You may have thyroid-related PCOS if you experience persistent fatigue, unexplained weight gain, hair thinning, cold sensitivity, dry skin, constipation, or irregular periods, especially if these symptoms don’t improve with typical PCOS strategies alone. This type is usually identified through thyroid lab testing (such as TSH, free T3, free T4, and thyroid antibodies). Also, it’s particularly important to address untreated thyroid issues, as they can make PCOS symptoms harder to manage.
Symptoms of PCOS
Reproductive and Fertility Symptoms
- Irregular menstrual cycles
- Missed or infrequent periods
- Very heavy or very light periods
- Lack of ovulation (anovulation)
- Difficulty getting pregnant
- Irregular or delayed ovulation
- Difficulty getting pregnant
- Poor egg quality
- Thickened uterine lining
- Implantation issues
- Recurrent miscarriage
- Reduced cervical mucus
Metabolic and Blood Sugar Symptoms
- Insulin resistance
- Sugar or carbohydrate cravings
- Fatigue after meals
- Difficulty losing weight
- Stubborn weight gain
- Central (belly) fat accumulation
Skin and Hair Symptoms
- Excess facial or body hair (hirsutism)
- Thinning scalp hair or hair loss
- Persistent adult acne
- Oily skin or scalp
- Darkened skin patches (acanthosis nigricans)
- Skin tags
Energy, Mood, and Mental Health Symptoms
- Chronic fatigue
- Brain fog
- Mood swings
- Anxiety or depression
- Low motivation or energy
Digestive and Inflammatory Symptoms
- Bloating
- Digestive discomfort
- Puffiness or fluid retention
- Joint or muscle aches
Can You Have PCOS Without Symptoms?
Yes! I often talk about “reversing PCOS” in my content. However, no matter what you do, you’ll always have PCOS. But, with the right lifestyle changes, you can naturally regulate hormones, ease inflammation, and increase insulin sensitivity. When you do this, the main drivers of PCOS symptoms disappear.
Even if you haven’t made a lot of changes, you may have fewer symptoms if you already have healthy eating, sleeping, and exercise habits. You’re already on your way to healing!
Complications of PCOS: Understanding Long-Term Risk
- Infertility or difficulty conceiving
- Endometrial hyperplasia
- Increased risk of endometrial cancer
- Increased risk for Type 2 diabetes
- Metabolic syndrome
- High blood pressure
- Elevated cholesterol
- Increased risk of heart disease
- Increased risk of stroke later in life
- Gestational diabetes
- Pregnancy-induced hypertension
- Sleep apnea
- Non-alcoholic fatty liver disease (NAFLD)
- Anxiety and depression (learn more about the link between PCOS, depression, and anxiety here!)
Treatment for PCOS: Natural Lifestyle Changes for Healing
The PCOS Weight Loss blog and our companion podcast, A Cyster and Her Mister, are all about holistically treating PCOS. No side-effect-heavy drugs, invasive procedures, or questionable trends—just a few strategic, natural, and research-backed changes to your daily life. For a full rundown, read our essential guide to managing PCOS naturally and download The Cysterhood app. There, you’ll find the resources you need to kickstart your healing journey!
Here’s each lifestyle change and how it can affect the root issues of PCOS:
| Lifestyle Change | Boosts Insulin Sensitivity | Eases Inflammation | Balances Hormones | Regulates cortisol (stress hormones) | Improves Brain–Ovary Communication |
| Gluten- and dairy-free diet | X | X | X | X | X |
| PCOS-friendly supplements (Inositol, berberine, etc.) | X | X | X | X | X |
| Reduced alcohol | X | X | X | X | |
| Limited caffeine | X | X | X | ||
| Hydration | X | X | |||
| Testosterone-balancing tea | X | X | X | X | |
| Slow-weighted workouts | X | X | X | X | X |
| Good Quality Sleep | X | X | X | X | X |
| Stress reduction and self-care | X | X | X | X | |
| Removal of endocrine-disrupting chemicals | X | X | X |
Should You See a Doctor for PCOS?
Yes. Definitely see a doctor if you suspect PCOS. I know it can be frustrating and, at times, difficult to get a provider to take your symptoms seriously. However, having medical support really matters.
A doctor can help confirm a diagnosis, rule out other conditions, check for potential complications, and monitor your health over time. You can also use these appointments to discuss supplements, lifestyle changes, and other therapies that may support your natural healing process.
What Doctor Treats PCOS?
- OB-GYN (Obstetrician–Gynecologist): Diagnoses PCOS, evaluates menstrual cycles and ovulation, orders pelvic ultrasounds, and manages period or fertility-related symptoms
- Endocrinologist: Treats hormone and metabolic imbalances, such as insulin resistance, high androgen levels, thyroid dysfunction, and adrenal issues
- Reproductive Endocrinologist: Helps women with PCOS who are trying to conceive, including ovulation support, egg quality concerns, and fertility treatments like IUI or IVF
- Primary Care Physician: Orders initial labs, monitors long-term health risks (diabetes, cholesterol, blood pressure), and coordinates care between specialists
- Registered Dietitian (PCOS-trained): Supports blood sugar regulation, inflammation reduction, and hormone balance through personalized nutrition and lifestyle strategies
- Functional or Integrative Medicine Doctor: Takes a root-cause, whole-body approach and often uses more comprehensive lab testing to identify underlying drivers of PCOS symptoms
- Mental Health Professional (Therapist or Psychologist): Helps manage the emotional, mental health, and stress-related impacts of PCOS
How Do Doctors Test for PCOS?
As I said earlier, no one test can definitively diagnose PCOS. Because of this, getting PCOS diagnosed can be a long and difficult process. Each type of doctor will also only have certain expertise and capabilities in terms of types of tests, so seeing multiple providers may be necessary. Here’s what they’ll look into:
- Medical history
- Symptom review
- Hormone blood testing
- Metabolic blood testing
- Pelvic ultrasound
A doctor will then review the results and diagnose you based on the Rotterdam Criteria. According to this framework, a woman has PCOS if she has two of the following symptoms:
- Irregular periods or absent periods
- Signs of excess androgens
- Polycystic ovaries
For more on detecting PCOS, read our post on how to get your hormone levels tested.
Does PCOS Ever Go Away?
No. Some people with PCOS assume it will go away after menopause, but that isn’t the case. While certain symptoms may improve, metabolic risks can actually worsen over time. And if you’re thinking hormonal birth control, Ozempic, or metformin are a cure for PCOS, you’d unfortunately be wrong there, too. Medications can help manage symptoms, but they don’t address the root causes of the condition.
You can actually learn more about medications and PCOS in my posts, “What Is Ozempic?” and “What Does Metformin Do for PCOS?”
That said, while PCOS doesn’t simply disappear on its own, it is reversible with intention and consistency. Targeted lifestyle changes—like eating to support hormone balance, exercising regularly, taking the right supplements, and prioritizing quality sleep—can make a huge difference. With each positive change, symptoms often improve one by one, until PCOS no longer runs your life.
For additional helpful information, make sure to visit my previous post, “How to Manage PCOS Symptoms Naturally.”
PCOS is a common hormonal and metabolic disorder in women of reproductive age.
PCOS is prevalent, complex, and far too often misunderstood—but it doesn’t have to control your life. If there’s one takeaway from all of this, it’s that your symptoms are real and they have real root causes. More importantly, there are natural, effective ways to manage symptoms once you understand what’s going on in your body.
The more informed you are about PCOS, the easier it becomes to advocate for yourself, target the right issues, and start healing—one intentional change at a time. You’re not broken, and you’re definitely not alone.
pcosweightloss.org (Article Sourced Website)
#PCOS #Symptoms #Diagnosis #Natural #Treatments
