The Achilles tendon is one of the most important connective tissues in your feet. Moreover, it’s the longest and strongest tendon in your entire body, connecting your calf muscles to the heel bone. In fact, it can withstand up to four times your body weight and allows plantar flexion of your feet — an essential movement allowing you to walk, run, and jump.1
However, experts are now noticing an uptick in Achilles tendon injuries from all walks of life. In a report from CNN, it’s not just professional athletes who are getting this injury. High-profile actors and ordinary people exercising at the gym have also torn their Achilles tendon.2 Numerous factors have been implicated in this issue, and a 2025 study shows that everyone, including you, could be at risk.
Data Confirms Achilles Ruptures Are Accelerating
A study published in The Orthopaedic Journal of Sports Medicine mapped out the rising rates in Achilles tendon ruptures in America. For the analysis, the researchers combed through data from 2001 through 2020. Specifically, they used the National Electronic Injury Surveillance System, a large federal database designed to track injury-related emergency visits across a representative sample of U.S. hospitals. This approach allowed the authors to estimate national trends rather than isolated regional snapshots.3
• The current state of Achilles tendon injuries — Across the study period, 235,189 emergency department visits for acute primary tendon ruptures were recorded. Among all tendon injuries, Achilles tendon ruptures stood out as the most common, accounting for 38.2% of cases. Other injuries included the biceps brachii (16.2%) and patellar tendon (12.7%).
• There is a clear, upward trend — The researchers calculated an average annual increase of about 3% in tendon rupture incidence over the 20-year analysis. Interestingly, that rise did not flatten out or reverse toward the end — it continued.
• A breakdown of risk by sex — Men experienced Achilles tendon ruptures at far higher rates than women, with an incidence rate of 2.46 per 100,000 person-years for men compared with just 0.48 for women. That translates to a male-to-female incidence rate ratio of roughly 5 to 1.
• Race-based differences — Black patients showed the highest overall incidence rate of tendon ruptures, at 4.78 per 100,000 person-years, compared with lower rates in White and other racial groups. The study did not specify an explanation for this gap, but it highlighted that tendon rupture risk does not distribute evenly across the population.
• Everyone could be at risk — A steadily rising injury rate over 20 years points to systemic drivers rather than isolated accidents. This means lifestyle changes, occupational demands, recreational exercise trends, and broader health factors likely shape tendon strength long before the rupture occurs. If you wait until pain forces you into an emergency room, the problem has already progressed too far.
The researchers also emphasized that the records were acute primary ruptures, not repeat injuries or complications from prior tears. That distinction matters because it shows the increase in injury rates does not come from poor recovery alone — it reflects a growing vulnerability in the population.
Mapping the Drivers Behind Achilles Rupture Risk
In a study published in the Journal of Orthopaedic Translation, researchers set out to identify why Achilles tendon ruptures continue to rise despite better awareness, training tools, and medical care. The researchers reviewed clinical evidence on rupture risk factors and prevention strategies, with a specific focus on how modern lifestyles affect tendon health.4
The paper focused on adults with Achilles tendon injuries across both athletic and non-athletic populations, reflecting real-world conditions rather than elite performers alone. The researchers also emphasized that ruptures increasingly affect people who exercise recreationally, work physically demanding jobs, or have metabolic disorders.
After analysis was complete, they noted that an Achilles tendon rupture is not a random event — it is the result of repeated tissue overload combined with biological weakening that goes unnoticed until failure occurs.
• Risk builds up long before pain appears — The researchers explained that many people develop silent tendon degeneration over time, meaning the tissue structure slowly weakens without obvious symptoms. This condition leaves the tendon vulnerable to sudden rupture during routine activity.
• Sudden changes in training patterns increase risk — Abrupt changes in physical load are a major driver of rupture risk. For example, sudden increases in running volume, intensity, or explosive movement place stress on the tendon fibers faster than they can repair.
• Foot and ankle mechanics also play a role — The authors described how abnormal foot alignment, limited ankle mobility, and poor force distribution increase localized strain within the Achilles tendon. Over time, this uneven stress degrades the collagen fibers.
• Metabolic health emerged as another overlooked factor — Conditions such as obesity, insulin resistance, and chronic inflammation impair tendon repair. Just like every other process in your body, the tendons also rely on steady nutrient delivery and efficient cellular repair. When those processes slow down, microscopic damage accumulates faster than your body fixes it.
• Drugs also weaken tendons — Certain drugs interfere with tendon cell function and collagen maintenance, making the tissue more fragile under normal loads. While the study didn’t go into detail about the mechanisms, it listed the following drugs as modifiable risk factors:
◦ Fluoroquinolones
◦ Antimicrobial drugs
◦ Statins
◦ Corticosteroids
◦ Aromatase inhibitors
◦ Anabolic steroids
◦ Isotretinoin
◦ Renin-angiotensin system drugs
◦ Thiazide diuretics and calcium channel blockers
• A comparison of compared modifiable and non-modifiable risk factors — Age, sex, and genetic structure fall outside your control, but training design, recovery time, metabolic support, and mechanical alignment do not. The review stressed that focusing only on unchangeable factors leads to missed prevention opportunities. In other words, the risk of injuring your Achilles tendon is something you can influence through choices, not chance or plain bad luck.
• The paper discussed why prevention often fails — Many people rely on pain as a warning sign, yet tendon degeneration progresses quietly. By the time discomfort appears, structural damage already exists.
• How tendon breakdown occurs at the microscopic scale — Collagen fibers lose organization, and enzymes that degrade connective tissue increase in activity. At the same time, oxidative stress rises inside tendon cells, reducing their ability to maintain strong fibers.
• Another mechanism involves blood supply — The Achilles tendon has limited circulation compared to muscle, which slows healing. When combined with metabolic strain or medication effects, this low blood flow leaves the tendon vulnerable. The researchers describe the process below:5
“[T]he middle Achilles tendon part is the least supplied with blood, relying on capillaries in the surrounding connective tissue for reperfusion. Under increased load, these areas are more prone to hypoxia and metabolic disturbances, leading to dystrophic changes.
Poorly supplied tendon parts exhibit higher temperature regimes, which increase the elastic component and significantly reduce tendon fiber strength.”
Could Taking Antibiotics Weaken Your Achilles Tendon?
As mentioned earlier, drugs are a factor in deteriorating tendon health. Now, a study published in the Journal of Sport and Health Science followed this angle, specifically investigating whether commonly prescribed oral fluoroquinolone antibiotics raised the risk of Achilles tendon injury compared with another widely used antibiotic, amoxicillin.6
The research team used a nationwide Danish health registry data in a nested case-control design, which means they compared people who experienced Achilles tendon lesions or ruptures with carefully matched individuals who did not. The goal was straightforward — determine how strong the association is, how quickly the risk appears after exposure, and whether dose matters.
• Risk quickly rises — Within the first 60 days after fluoroquinolone use, the risk was 3.6 times higher in the two months after taking the drug compared to amoxicillin. Even at 90 days, the risk remained high at 2.74, and in one year it stayed elevated at 1.49.
• The impact of dosage — The researchers measured cumulative defined daily doses, which reflects how much of the antibiotic a person consumed over time. Individuals who accumulated more than 10 defined daily doses had a significantly higher risk of Achilles tendon injury than those with lower exposure. This means that longer or repeated courses raise risk more than a short exposure, especially if prescriptions stack up over time.
• What happens when other medications enter the picture — People who experienced Achilles injuries more often have recent exposure to oral glucocorticoids compared with controls. Specifically, about 6% of cases had used glucocorticoids versus 2% of controls. Thus, if you’re an athlete taking both antibiotics and steroids within a short window, your Achilles tendon faces further increased risk.
• How fluoroquinolones affect tendon tissue directly — These drugs interfere with collagen synthesis, meaning they disrupt the process by which tendon cells maintain and repair their structural fibers. Collagen acts like tightly woven rope strands and when these weaken, the tendon loses tensile strength.
• Beware of antibiotics on your connective tissues — By quantifying how strongly and how quickly fluoroquinolones raise Achilles tendon rupture risk, this research adds a critical piece to the larger picture. It shows that modern injury patterns do not stem only from movement or training habits. Sometimes, the trigger comes from a prescription, quietly weakening tissue until the tendon reaches its breaking point.
Some Tips to Protect Your Achilles Tendon
Going back to the CNN report, it’s noted that everyone who is 35 to 50 years old can tear their Achilles tendon. However, there are several things you can do to lower the risk:7
• Get enough rest — After a strenuous game or exercise session, give your body enough time to recover, especially if you’ve been using your legs a lot.8 This tactic allows your tissues to adapt and preventing overuse injuries.9
• Gradually increase intensity — Slowly ramping up exercise intensity, coupled with proper rest, helps lower the risk of injuries.10
• Buy good shoes — Many people overlook the importance of proper footwear when it comes to preventing injuries. According to a study published in the Clinical Journal of Sport Medicine, high-top shoes can significantly reduce tension in the Achilles tendon compared to low-top shoes.11
In another study, shoes biased to forefoot landing was found to improve Achilles tendon loading, “and may be useful for progressing loading prior to introducing more advanced movements.”12
• Reduce vegetable oil consumption — As noted earlier, metabolic disorders have been identified as a risk factor, which is likely influenced by a diet high in linoleic acid (LA).
LA affects your overall metabolic health and ability to produce healthy cellular energy. That said, keep your intake to below 2 grams per day from all sources, such as soybean, cotton, and safflower oil. In addition, avoid ultraprocessed foods, as these also contain LA. Next, add in healthy fat sources, such as coconut oil and grass fed tallow or ghee.
To help monitor your intake, sign up for the upcoming Mercola Health Coach app. It contains the Seed Oil Sleuth, which helps monitor your LA intake to a tenth of a gram.
Support Your Achilles Tendon with Collagen
Collagen is the main structural protein found in your skin, tendons, and bones, as well as playing a crucial role in many bodily functions.13 Thus, proper collagen intake is essential to keeping your Achilles tendon strong and flexible, especially if you’re a high-level athlete or fitness enthusiast.
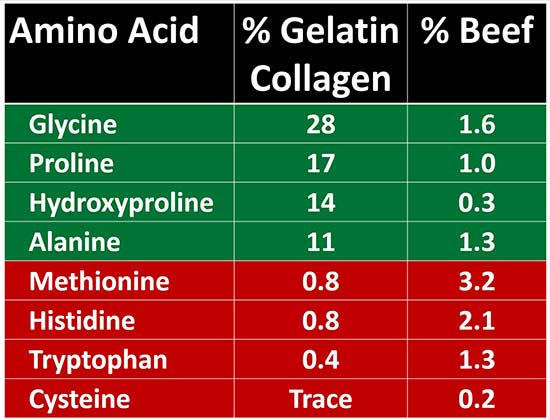
• A primer on collagen sources — For your body to produce collagen, your body will need the right amino acids from animal parts that have them. That’s because red meat alone won’t give your body the amino acids (highlighted in green below). In addition, a high intake of amino acids from red meat (highlighted in red below) can promote inflammation, as well as suppress thyroid function and metabolism.14
• Ideal collagen intake — I recommend that a third of your overall daily protein intake comes from collagen sources, as 30% of your body is comprised of this protein.
• Best source of collagen — For your body to make enough collagen, I recommend making your own bone broth using organic, grass fed animal bones. Gelatinous cuts of meat also work, and you can use slow-cooking or pressure-cooking to make them easier to eat. To learn how to make your own bone broth, read “The Ultimate Guide to Bone Broth: Nature’s Collagen Supplement.”
Frequently Asked Questions About Achilles Tendon Ruptures and Injuries
Q: Why are Achilles tendon injuries becoming more common?
A: Achilles tendon ruptures have increased steadily over the past two decades due to systemic factors like lifestyle changes, recreational exercise trends, metabolic health issues, and cumulative tissue overload, not just sports-related accidents.
Q: Who is most at risk for an Achilles tendon rupture?
A: Men face significantly higher risk than women, Black patients show higher incidence rates, and adults aged 35 to 50 are especially vulnerable, though rising trends suggest most people are at risk.
Q: Can Achilles tendon damage develop without warning signs?
A: Yes. Tendon degeneration often occurs silently over years, weakening collagen structure without pain, making sudden rupture possible during routine activities before any symptoms appear.
Q: Do medications affect Achilles tendon strength?
A: Certain drugs, especially fluoroquinolone antibiotics and corticosteroids, impair collagen synthesis and tendon repair, sharply increasing rupture risk shortly after use, particularly with higher or repeated doses.
Q: What steps can help protect the Achilles tendon?
A: Gradual training progression, adequate recovery, proper footwear, minimize LA intake, avoid antibiotics, and sufficient collagen consumption from natural sources like bone broth can strengthen tendon resilience and reduce injury risk.
articles.mercola.com (Article Sourced Website)
#Achilles #Tendon #Injuries #Rising #Among #Athletes
